
Best Antibiotic for Otitis Media to Adults 20+The most frequent pediatric infection for which antibiotics are administered in the US is acute otitis media (AOM), which mostly affects children [1, 2]. The vast majority of medical literature is devoted to the diagnosis, treatment, and side effects of pediatric AOM, and a great deal of what we know about AOM in adults has been extrapolated from research in children.
The etiology, diagnosis, and management of AOM in adults will all be covered in this article. Separate topics are covered in relation to AOM and other typical middle ear pathologies in children. (See also “Acute otitis media in children: Clinical manifestations and diagnosis,” “Acute otitis media in children: Epidemiology, microbiology, and complications,” “Acute otitis media in children: Treatment,” “Otitis media with effusion (serous otitis media) in children: Clinical features and diagnosis,” and “Otitis media with effusion (serous otitis media) in children: Management.)
Adult chronic otitis media (COM) evaluation and treatment are also covered individually. (Read more about adult cases of chronic otitis media, cholesteatoma, and mastoiditis.)Best Antibiotic for Otitis Media to Adults-(20+)
An acute, suppurative infectious condition known as acute otitis media (AOM) is characterized by inflammation of the mucosa lining the middle ear cavity and the presence of infected middle ear fluid (picture 1). The infection is most usually brought on by the Eustachian tube’s diminished function, which causes the retention and suppuration of residual secretions (figure 1). If the tympanic membrane is perforated, AOM may also be related to purulent otorrhea. AOM often responds quickly to antibiotic treatment
Best Antibiotic for Otitis Media to Adults 20+
EPIDEMIOLOGY OF ACUTE OTITIS MEDIA
The frequency of AOM considerably decreases after age 5 and is most common in infants between the ages of 6 and 24 months [1,3]. In children under the age of five, the annual incidence of AOM was estimated to be between 45 and 60 percent; in children aged 5 to 14 years, between 19 and 22 percent; in children and adults aged 15 to 24 years, between 3.1 and 3.5 percent; and in adults aged 25 to 85 years, between 1.5 and 2.3 percent [4]. Based on the results of this investigation, the prevalence of AOM among adults in resource-rich countries is probably less than 1%.
The incidence of AOM and otitis media with effusion (OME) was 2.7 and 1.4 per 1000 person-years, respectively, in a 2014 to 2018 survey of adult outpatient visits to United States Veterans Administration medical clinics [5]. The incidence of AOM was 5.3 per 1000 person-years overall in a 2015–2018 Netherlands study that included patients under the age of 15; the incidence decreased with age (age 15 to 39, 7.1 per 1000 person-years; age 64 years, 2.7 per 1000 person-years) [6].
Over the past 20 years, there has been a decrease in the incidence of AOM among children in the United States. Between 1995 and 2006, the number of outpatient visits and antibiotic prescriptions for AOM in children under the age of five decreased by one-third in the United States [7]. Additionally, there was a drop in visits for AOM in children under the age of seven from 2001 to 2011, and this decline was particularly quick in children under the age of two from 2010 to 2011 [8].
This decrease in incidence may be brought on by the introduction of standard pneumococcal vaccination in babies. The 13-valent pneumococcal vaccine (PCV13) took the place of the 7-valent pneumococcal vaccine (PCV7) in the United States in 2010.
Other nations have also noticed a decline in the incidence of AOM, which may be connected to the introduction of the pneumococcal vaccine. For instance, in Sweden, the incidence of AOM decreased by 21% in children aged 5 to 17 and by 42% in children under the age of 5, respectively, after the introduction of the universal pneumococcal vaccine for newborns in 2009 [9]. (See “Pneumococcal Vaccination in Children” and “Impact of Pneumococcal Conjugate Vaccines on Infant Immunization in the United States”).Best Antibiotic for Otitis Media to Adults-(20+)
Related Read;Top 10 Best Medical Schools in Japan
MICROBIOLOGY
Although cultures of middle ear fluid obtained by needle aspiration (myringotomy) in children have provided the majority of the data on the microbiology of acute otitis media (AOM), the microbiology of AOM in adults is comparable to that seen in the pediatric population.
Streptococcus pneumoniae and nontypeable Haemophilus influenzae are the most prevalent bacterial infections in children, with Moraxella catarrhalis ranking third [3,10]. Globally, M. catarrhalis was responsible for 3 to 14% of pediatric AOM cases, while S. pneumoniae and H. influenzae together caused 50 to 60% of them [11]. Although Staphylococcus aureus may be a significant pathogen in adults based on limited investigations, Group A streptococcus and Staphylococcus aureus are less frequently found causes of AOM in general pediatric populations. In patients with severe AOM who need to be hospitalized, Group A streptococcus may also be a significant pathogen [12,13]. Typical studies consist of:
A 1991 study of the myringotomy samples of 34 adults with AOM reported the major pathogens to be nontypeable H. influenzae (26 percent), S. pneumoniae (21 percent), M. catarrhalis (3 percent), Group A streptococcus (3 percent), and S. aureus (3 percent) [14].
●A South Korean study analyzing middle ear fluid from a mixed adult and pediatric population with AOM and spontaneous tympanic membrane perforation revealed the major pathogens to be S. aureus (21 percent, including methicillin-resistant S. aureus [MRSA] in 4 percent), S. pneumoniae (16 percent), Pseudomonas species (8 percent), H. influenzae (5 percent), and Klebsiella (5 percent) [12]. Coagulase-negative staphylococci were isolated in 24 percent of cultures, however, suggesting possible contamination by ear canal flora.
●In 60 adults with severe AOM requiring hospitalization, almost 50 percent were culture-negative, while culture-positive cases demonstrated Group A streptococcus (15 percent), S. pneumoniae (10 percent), Pseudomonas (8 percent), and S. aureus (5 percent) [13]. The source of culture (fluid from perforated tympanic membrane versus myringotomy) in this study was not reported.Best Antibiotic for Otitis Media to Adults-(20+)
Most common causative organisms:
Streptococcus pneumoniae;-One of the most significant bacterial causes of AOM is S. pneumoniae. Studies on the pneumococcal serotypes most likely to cause AOM in adults are lacking, but since the introduction of the 7-valent and 13-valent pneumococcal vaccines, there has been a discernible shift in the causal serotypes in children (PCV7 and PCV13). (For more information, see the section on the “Effect of baby immunization” in “Acute otitis media in children: Epidemiology, microbiology, and consequences.”)
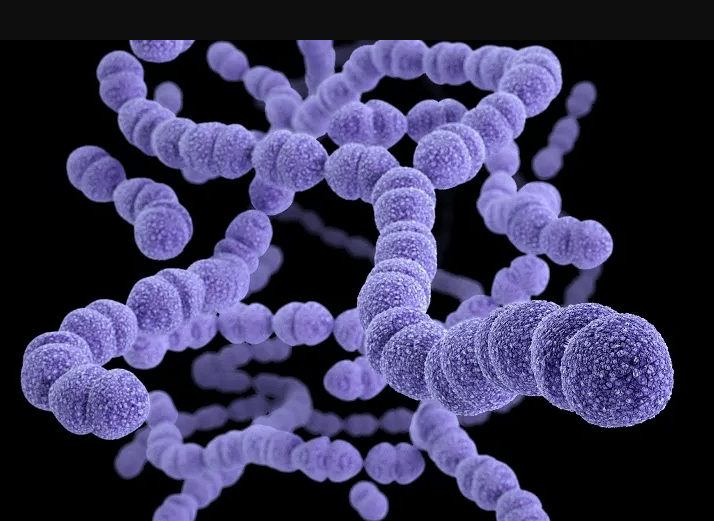
Depending on age and/or coexisting medical problems, the Centers for Disease Control and Prevention (CDC) advises immunization with PCV13 and the 23-valent pneumococcal polysaccharide vaccine (PPSV23) for adults. Pneumococcal vaccinations are expected to have some protective effects, even though there are no data comparing the prevention of AOM in adults to that in children. Adult vaccination administration recommendations are covered elsewhere. (See “Adult pneumococcal vaccine.“)Best Antibiotic for Otitis Media to Adults-(20+)
Haemophilus influenzae ;-AOM due to H. influenzae in patients of all ages is due to nontypeable strains in the majority of patients
Moraxella catarrhalis ;-M. catarrhalis is responsible for 3 to 14 percent of AOM in children and is the third most common otopathogen [11]. High-quality data in adults are more limited, but in one study M. catarrhalis caused 3 percent of adult AOM cases [14].
Staphylococcus aureus ;-Children seldom get AOM from S. aureus, especially methicillin-resistant strains. Adults may be more susceptible to it as a cause of AOM, however the actual incidence is unknown. S. aureus has been linked to prolonged otorrhea after tympanostomy tube implantation in individuals with chronic suppurative otitis media (CSOM).
Group A streptococcus;-Prior to the development of antibiotics, Group A streptococcus was a substantial contributor to severe middle ear illness, frequent tympanic membrane rupture, and mastoiditis, which were all symptoms of AOM [16,17]. Although the origin of Group A streptococcus’ decreased frequency as an AOM cause is unknown [18], Although it can be particularly fulminant when it does, Group A streptococcal AOM in adults is the most typical cause of severe AOM necessitating hospitalization, according to one study [13].Best Antibiotic for Otitis Media to Adults-(20+)
Viral pathogens:
Children who have viral upper respiratory infections are frequently predisposed to AOM, and viruses and bacteria can both infect the middle ear [19]. Although there aren’t many research on the adult population, this is probably also true for adults. Rhinovirus and respiratory syncytial virus were the most often discovered viruses in investigations using reverse transcription polymerase chain reaction (RT-PCR) in children; parainfluenza, coronavirus, and adenovirus were also sporadically identified [20]. Since the start of the coronavirus disease 2019 (COVID-19) pandemic, a number of investigations in adults have documented cases of AOM in COVID-19 patients; in some cases, the etiologic virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was found in the middle ear fluid [21–23].
Less common or rare causative organisms:
- Mycoplasma pneumoniae-Although the etiologic significance of M. pneumoniae in the AOM is unclear, some patients with lower respiratory tract infections caused by M. pneumoniae also have concurrent AOM. There aren’t many studies on M. pneumoniae in adult AOM. 4 percent of middle ear fluid samples from children with AOM in a Finnish research tested positive for M. pneumonia, although majority (69 percent) of these M. pneumoniae-positive samples also tested positive for a characteristic AOM pathogen (M. catarrhalis, S. pneumoniae, or H. influenzae) [24].
- Rare causes include diphtheritic otitis, tuberculous otitis, and otogenous tetanus, and otitis media due to Chlamydia trachomatis.
PATIENT FACTORS CONTRIBUTING TO THE DEVELOPMENT OF ACUTE OTITIS MEDIA
A predisposing factor for the development of acute otitis media can be eustachian tube dysfunction, entities producing Eustachian tube compression or outlet obstruction, or an aberrant host immune response (AOM).
-Eustachian tube dysfunction-The primary cause of middle ear infections in both children and adults is dysregulation of the eustachian tube (figure 1). The absence of aeration and fluid buildup in the middle ear space caused by eustachian tube dysfunction create an environment that is favorable for the development of AOM or otitis media with effusion.
The patency of the Eustachian tube is improved by anatomical changes that occur during adolescence, specifically the fall of the soft palate muscle sling relative to the opening. With age, the incidence of AOM declines due to this anatomical shift. Eustachian tube dysfunction, however, can continue until adulthood and cause AOM to happen at any age.
Eustachian tube obstruction –Anything causing external compression of the Eustachian tube, or obstruction of the Eustachian tube or of its outlet, can also predispose to AOM, particularly unilateral AOM. Examples include malignancy (ie, lymphoma, nasopharyngeal carcinoma) and post-radiation fibrosis.Best Antibiotic for Otitis Media to Adults-(20+)
Immune dysfunction –
Any irregularity in the respiratory mucosal membrane, which covers the mastoid air cells, middle ear cavity, and Eustachian tube, acts as an immunologic protective barrier, raising the possibility of infection.
The respiratory epithelium produces more mucus, which contains the powerful antibacterial enzyme lysozyme, in response to any illness [25]. Increased mucus production is accompanied by mucosal blood vessel dilation, which attracts white blood cells and antibodies to the region and strengthens the mucopurulent protective layer.
Additionally, the respiratory epithelium has motile cilia that aid in secretion mobilization. Ciliary dyskinesia may cause mucociliary clearance to be ineffective, which could compromise the proper operation of this crucial host immune defense. [26,27]
PRESENTATION AND DIAGNOSIS
Making a correct diagnosis of acute otitis media (AOM) is crucial to preventing overtreatment with the wrong antibiotic medication. Making the right diagnosis requires meticulous otoscopic examination and evaluation of the patient’s clinical presentation.
Also You May Read;Top 10 healthcare companies in India
Clinical manifestations-
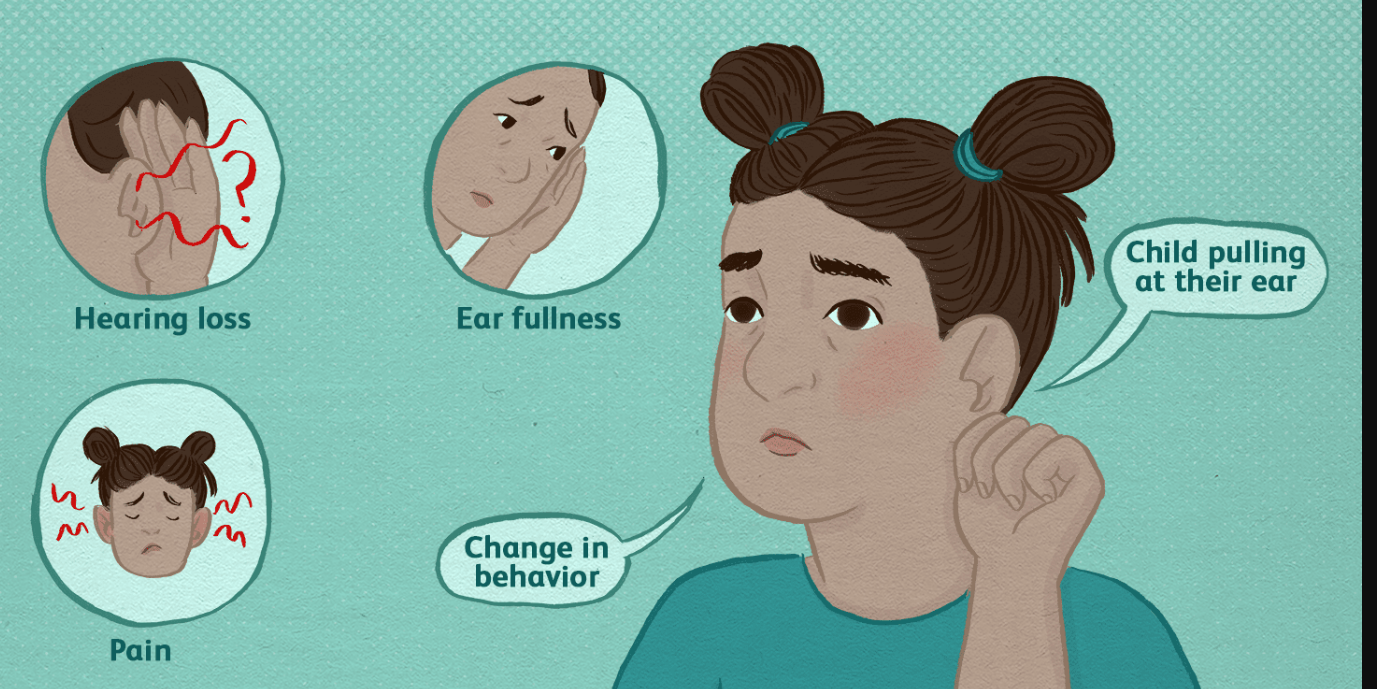
A seasonal allergic rhinitis flare-up or upper respiratory tract infection commonly occur before the onset of AOM in adults. Adult AOM is often unilateral and is accompanied by hearing loss or muffling as well as otalgia (ear pain). There are several levels of pain that might exist. The patient may experience an abrupt reduction of discomfort, potentially followed by purulent otorrhea, if the tympanic membrane has burst.
Even though dysequilibrium is occasionally mentioned, it may exist. The conductive hearing loss that could result from middle ear fluid is typically temporary.
Other signs and symptoms include a high fever, excruciating ear ache, or facial paralysis point to uncommon problems
Diagnosis with otoscopy
In adults with suspected AOM, the diagnosis is confirmed by the presence of typical features on otoscopic examination
Key features include:
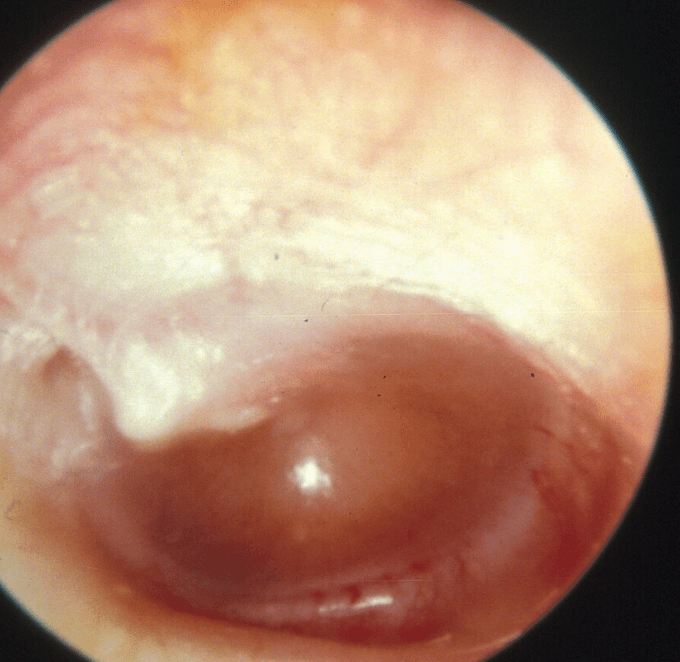
- Bulging tympanic membrane
- Reduced mobility of the tympanic membrane when pneumatic pressure is applied (if pneumatoscopy is available)
- Partial or complete opacification of the tympanic membrane
- Erythema of tympanic membrane
Examination with a handheld otoscope is essential for an accurate diagnosis of AOM. The addition of pneumatoscopy allows evaluation of tympanic membrane motion and is therefore also recommended for diagnosis. Otomicroscopy, generally available only in otorhinology specialty practices, permits even greater visualization of the tympanic membrane.
Examination typically demonstrates tympanic membrane bulging, opacification, erythema (picture 1), and poor mobility when pneumatic pressure is applied using a pneumatic otoscope . A normal tympanic membrane is translucent (picture 3). (picture 3). By contrast, when there is fluid in the middle ear, the tympanic membrane appears cloudy, yellowish, or opaque. When there is an air-fluid level present, the tympanic membrane appears translucent above and opaque below the line of demarcation If there is an associated tympanic membrane rupture, there may be a visible perforation and possibly purulent material in the ear canal.Best Antibiotic for Otitis Media to Adults-(20+)
Some patients with suspected AOM may have a significant amount of cerumen partially or completely obstructing the ear canal, preventing adequate evaluation of the tympanic membrane. For these patients, we advise cautious removal of the obstructing material with either gentle curettage or aspiration under direct visualization. When AOM is a concern, removal of cerumen via irrigation should always be avoided because of risk of tympanic membrane rupture. If the obstructing cerumen cannot safely be relieved via curettage or aspiration, referral to otorhinology is appropriate.
The predictive value and accuracy of abnormal otoscope findings has been studied in children but has not been reported for adults with AOM [29-31]. In a pediatric population, the triad of a bulging tympanic membrane, impaired mobility, and redness or cloudiness of the tympanic membrane predicted the diagnosis of AOM, confirmed with myringotomy, in 83 to 99 percent of cases (table 1) [31]. In another study, a bulging tympanic membrane was more predictive of AOM than a red tympanic membrane [29].
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of acute otitis media (AOM) includes otitis media with effusion (OME) chronic otitis media (COM), external otitis (otitis externa), herpes zoster infection, and other deep space head and neck infections.
Otitis media with effusion-OME is a condition that is frequently clinically mistaken for AOM in adults (figure 2). The presence of middle ear fluid without immediate symptoms of a bacterial infection or disease is what characterizes OME. OME may occur before or after an episode of AOM and can be brought on by a recent viral infection, barotrauma, or allergies. Dysfunction of the eustachian tube is frequently a risk factor. Rarely, OME is brought on by a mass, such as nasopharyngeal carcinoma or another cancer, blocking the Eustachian tube opening in the nasopharynx, or as a result of radiation therapy for nasopharyngeal malignancy. In order to rule out obstructive pathology, nasopharyngoscopy and perhaps computed tomography (CT) should be performed in every instance with recurrent, unilateral otitis media with effusion.
Chronic otitis media –
When a subacute or chronic tympanic membrane perforation takes place alongside a chronic ear infection or recurring infections, COM is diagnosed.
Tympanic membrane perforation without concomitant drainage is a defining feature of benign COM.
There is continuous, often straw-colored serous leakage through the perforated tympanic membrane in COM with effusion (or chronic serous otitis media).
Chronic purulent drainage via the ruptured tympanic membrane is the hallmark of chronic suppurative otitis media (CSOM).
Some otologists identify COM alternatively based on the existence of a cholesteatoma or a chronic tympanic membrane perforation (referred to as “COM mucosal illness”) (“COM benign squamous disease”). If there is otorrhea, the phrase “active” is also used, and if it is dry, the term “inactive.”
Bullous myringiti-
— Bullous myringitis is an infectious condition in which blisters (bullae) or vesicles develop on the tympanic membrane. The disorder may mimic AOM with a thickened and erythematous tympanic membrane, but the pathologic process is limited to the tympanic membrane and does not affect the contents of the middle ear. Compared with AOM, bullous myringitis may be particularly painful.Best Antibiotic for Otitis Media to Adults-(20+)
The etiology is unknown, but it is believed to be viral. In studies published over 50 years ago, experimental infection of adult volunteers with M. pneumoniae resulted in hemorrhagic bullous myringitis [40]. However, subsequent studies of bullous myringitis have not identified M. pneumoniae as a causative agent.
TREATMENT OF ACUTE OTITIS MEDIA
Antibiotics are the mainstay of treatment of uncomplicated acute otitis media (AOM) in adults, and initial antibiotic choice is determined by knowledge of the most common causative pathogens.
At least 25% of AOM cases in children can be attributed to viral respiratory pathogens, and certain AOM episodes can be treated without the use of antibiotics. For certain kids with modest symptoms, the American Academy of Pediatrics and the American Academy of Family Physicians recommend initial observation in the United States. [41]
Duration of therapy-We administer antibiotics for five to seven days for mild to moderate infections and a 10-day treatment for more severe infections (defined as major hearing loss, severe discomfort, and/or notable tympanic membrane erythema). High-quality data about the ideal length of therapy are missing. Patients with severe AOM and systemic symptoms can need more intense first care, such as middle ear fluid and blood cultures, as well as initial intravenous antibiotic therapy.
Management of acute tympanic membrane rupture in acute otitis media –
The vast majority of acute tympanic membrane perforations brought on by AOM will naturally heal. When it happens, the perforation enables the discharge of infected fluid, alleviating middle ear pressure and promoting faster healing of the highly vascularized tympanic membrane. There is no evidence to suggest that treating individuals with AOM with a perforated tympanic membrane with a topical antibiotic in addition to oral antibiotics alone is superior in either pediatric or adult patients.
Some UpToDate authors treat patients with AOM and acute tympanic membrane rupture using topical antibiotic ear drops in addition to oral antibiotics, whilst other authors only use oral antibiotics.Best Antibiotic for Otitis Media to Adults-(20+)
If a topical antibiotic is used, we select one with no known ototoxicity (e.g., we stay away from preparations that contain aminoglycosides) and treat for 7 to 10 days.
Frequently Asked Questions
Acute otitis media treatment Adults with uncomplicated acute otitis media (AOM) are treated mostly with antibiotics, and the initial antibiotic used depends on knowledge of the most prevalent bacteria that cause AOM.
- What is the best antibiotic for ear infection in adults?
Only ofloxacin (Floxin Otic and generic) or the more costly combination drug ciprofloxacin-dexamethasone should be used as eardrops for bacterial infections (Ciprodex).
- What is the first-line treatment for otitis media?
Amoxicillin at a dosage of 80 to 90 mg per kg per day should be the first-line antibiotic for most children with acute otitis media. Patients with otitis media who fail to respond to the initial treatment option within 48 to 72 hours should be reassessed to confirm the diagnosis
Another name for a middle ear infection is otitis media. It denotes a bacterial infection beneath the eardrum. Any disease that prevents middle ear fluid from draining can lead to this type of ear infection. Allergies, a cold, a sore throat, or a respiratory infection are some of these conditions.
Be the first to comment